I’ve written about the impact of climate, global or local, on the transmissibility of COVID-19 on several occasions, e.g., here and here. A new study in Nature Communications brings a great deal of the early findings into perspective.
The study considered meteorological data from March 15 to December 31 of 2020, capturing 19.5 million cases of COVID-19 over 2,669 counties in the US – both a relatively long timeframe and reasonably “granular” data, neither too aggregated nor too local. The climate data were simply temperature, humidity (the amount of water in the air), and surface UV radiation.
The choice of what measure of COVID-19 to use has provided varying results in the studies generated over the last year. Cases are not the same as hospitalizations or deaths, and there are always the asymptomatic who blurred the precision of our measures. The researchers chose to use Rt, “the mean number of new infections caused by a single infected person, given the public health measures in place, in a population in which everyone is assumed to be susceptible.”
Their calculation of an Rt involved consideration of our mobility: commuting from work, doing errands, and just “getting out.” They also considered that mobility changes over the day, fewer of us are out after, say, midnight than at noon. In any instance, Rt gives us a sense of how transmissibility changes when there is little change in who might be susceptible – it allows us to more clearly see, in this instance, the impact of climate, but not perfectly.
Generalizations about our climate
- Southern counties were hotter than northern counties
- In the east, southern counties were more humid than northern ones; the west was less humid, and this was more pronounced inland than along the coast.
- Southern counties had more UV exposure than northern ones
The relation of those variables to COVID-19 transmission
The researchers next determined which combination of temperature, humidity, and UV exposure resulted in the lowest Rt, COVID-19’s changing transmissibility.
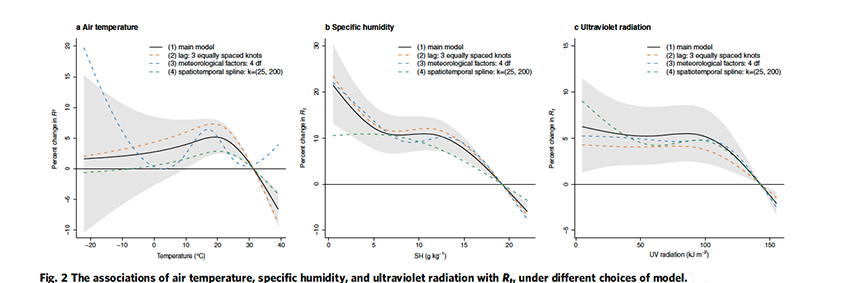
None of these patterns were linear, making their interactions less linear, that is, more complex.
- From 68 to 104°F, lower temperatures were associated with increased transmission. The “optimum” was 88°F, and the association was lost below 50°F, when presumably more of us were moving indoors.
- Humidity had a “stable range,” but on either side of that, higher humidity was associated with decreased transmission. Of the three factors, changing humidity had the most significant impact. [1]
- UV radiation had no impact upon transmission until it rose above a certain level, and then increasing UV radiation was associated with decreasing transmission. [2]
The researchers attributed [3] 3.7% of transmissibility to temperature, 9.35% to humidity, and 4.44% to UV radiation – overall, the climate had ~17.5% impact upon how transmissible COVID-19 was at any given time. In the study’s sensitivity analysis, which considers how other variables might influence the calculated outcomes, demographics, socioeconomics, smoking, obesity, and air pollutants had little impact.
PM2.5
Dr. Lipfert, a member of our Board of Scientific Advisors, has written extensively on the relationship between COVID-19 and PM2.5. He has long felt that it was not, despite the opinion of the New York Times, a causal factor in COVID-19 deaths. This study lends support to his interpretation of the data. The researchers found that PM2.5 was a confounder of the effect of temperature. In essence, while studies reported on PM2.5, they saw the unmeasured, and therefore the unconsidered, impact of temperature. Transmissibility of COVID-19 still tracked for humidity and UV radiation when PM2.5 was taken into account, making them “more robust predictors than temperature.”
Another of Dr. Lipfert’s points, that we spend so much time indoors, was also “channeled” by the researchers. They pointed out that while we can and do alter our indoor temperature, we infrequently change our indoor humidity, which “closely mirrors outdoor levels, perhaps explaining why ambient outdoor [humidity] is more strongly associated with [COVID-19] transmission than ambient outdoor temperature.”
For a seasonal respiratory virus, colder, drier, and lower UV radiation all “promote” viral transmission. We have seen it with seasonal flu, and we see it again with COVID-19. The association is not a one-to-one correspondence, the interactions are entangled, but it seems that humidity is another way we might further protect ourselves moving forward.
[1] Humidity is one of those measures that is difficult, at least for me, to explain – like pornography, I know it when, in this case, I feel it. Specific humidity is a close approximation to what we feel when we go outside. Higher humidity makes it feel muggier.
[2] UV radiation may play a dual role, lessening the viability of the virus and increasing our Vitamin D exposure, an important nutrient in our immune response
[3] The attributable amount or factor is a mathematical exercise in which the optimum values of temperature, humidity, and UV exposure are used to calculate the excess number of cases over 14 days, and then the data are smoothed. Is it exact? No. Is it in the ballpark? Perhaps, but it is a reasonable best guess.
Source: Role of meteorological factors in the transmission of SARS-CoV-2 in the United States Nature Communications DOI: 10.1038/s41467-021-23866-7




