That's a good question. Masks remain one of the non-pharmaceutical means of controlling the spread of infection. But how effective has COVID masking been in practice?
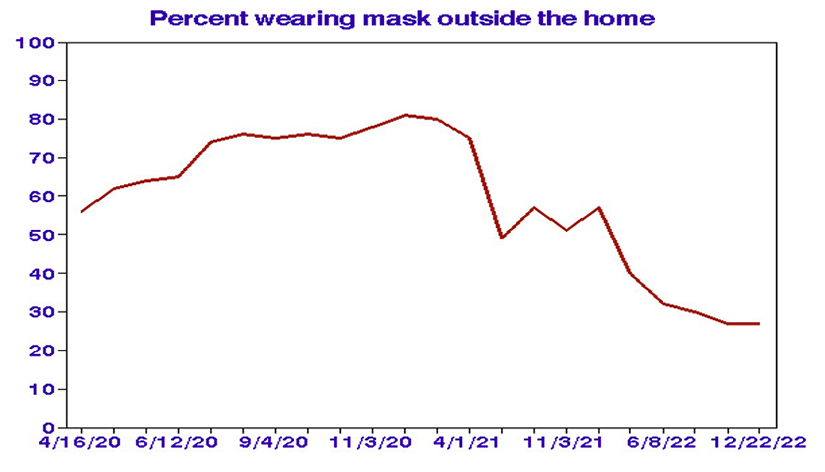
To address this fundamental question, I considered state-level data on frequencies of wearing a mask outside the home [1], which increased to a peak in late 2020 following and then declined substantially until recently.
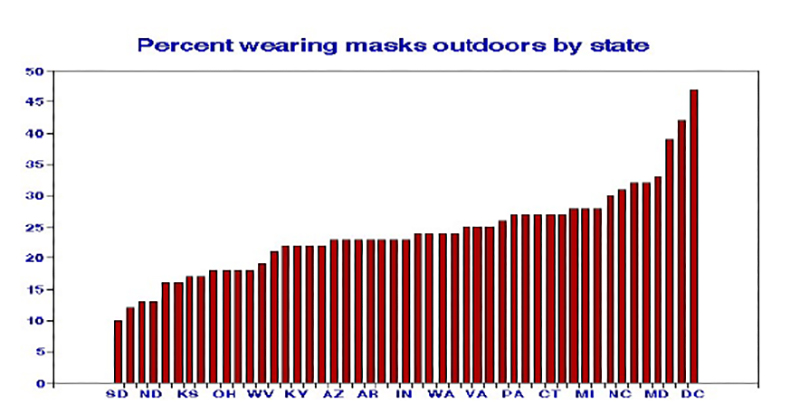
 I then considered the distribution of masking frequencies among the 48 contiguous states and the District of Columbia. While averaging 24%, masking was much less common in western states and more so in the East.
I then considered the distribution of masking frequencies among the 48 contiguous states and the District of Columbia. While averaging 24%, masking was much less common in western states and more so in the East.
We have previously shown that COVID-19 outcomes may be affected by various personal and demographic variables. Here I used linear regressions to estimate the relationships between those variables and masking based on differences among states from 2020 to 2023.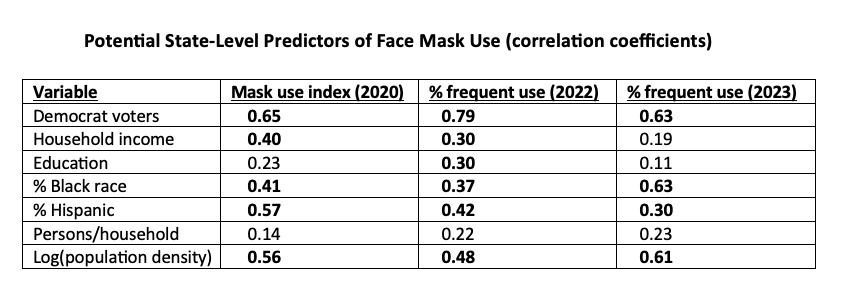 Bold-face correlation coefficients are statistically significant at the 0.05 level.
Bold-face correlation coefficients are statistically significant at the 0.05 level.
- Most of the correlations are consistent over time.
- Political affiliation shows the strongest relationships.
- Decisions to mask are not random.
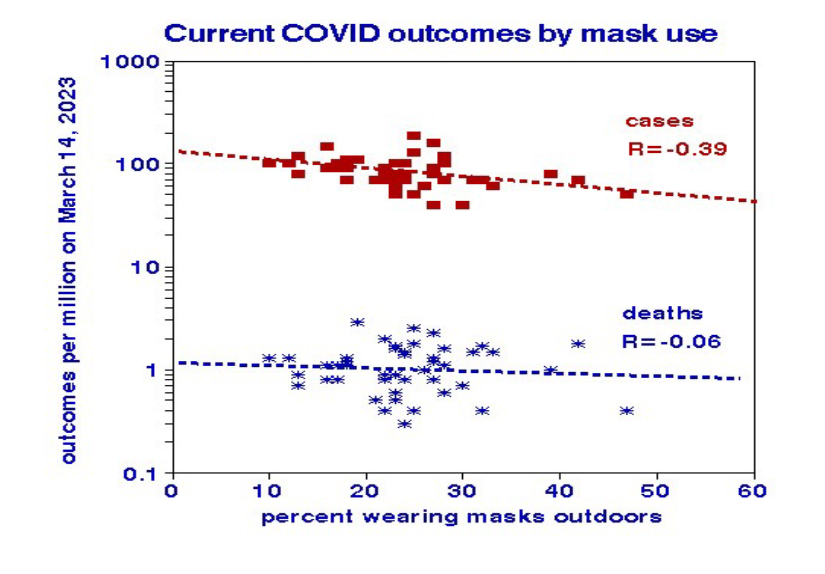
Based on daily 7-day average outcomes in March 2023, outdoor masking offered significant relief from infection but not from death. If 100% outdoor masking could be achieved, COVID-19 daily cases could be reduced to about 22 per million, far fewer than typically experienced from influenza, for example.
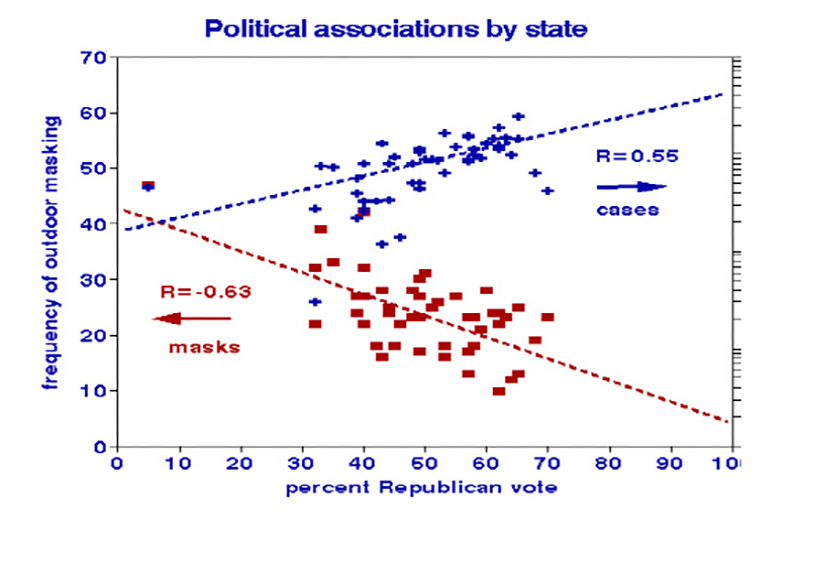
 I also investigated political relationships using the 2020 national election votes and found that relationships with masking and infection are mirror images.
I also investigated political relationships using the 2020 national election votes and found that relationships with masking and infection are mirror images.
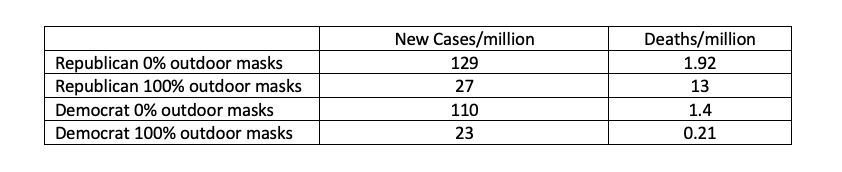
 Because both masking and politics can be significant predictors of COVID-19 outcomes, I postulated a 2-predictor regression model based on frequencies of outdoor masking and political affiliation and developed the following estimates:
Because both masking and politics can be significant predictors of COVID-19 outcomes, I postulated a 2-predictor regression model based on frequencies of outdoor masking and political affiliation and developed the following estimates:
My underlying assumption in this assessment is that the decision to wear a mask is not motivated by perceived need. Some people may wear masks more often out of a sense of social propriety, not because they consider themselves more vulnerable.
Underlying health status (such as comorbidity, an indicator of COVID vulnerability) is a potentially essential but unobserved latent variable. [2] Masking only the vulnerable portion of a population would confer the most benefit; masking only the immune would have little or even negative benefits. The benefit of vaccination in a given state depends on the fraction of vulnerables, and any potentially confounding variables that describe such vulnerability could thus be necessary.
Only about 1% of COVID cases die within a few weeks, implying that the most vulnerable subpopulation of a state (for which we have no data) may be quite small. However, in a bivariate state-level analysis, I found that Republican deaths were about 5-fold higher than Democrat, masked or not; the strength of that relationship appears to overwhelm other factors.
After all this number crunching, what to conclude about mask effectiveness in the general public?
The association of statewide COVID infection rates with masking is statistically consistent but modest. Nevertheless, any prevented infections reduce hospitalizations, deaths, and long-COVID cases. Failure to find direct mortality relationships may be due to the study's observational nature, uncertainties in the relatively small daily death counts, failure to consider other indoor masking venues [1], or differences in underlying health conditions.
When in doubt, mask!
[1] “Masking outside the home” was the only available state-level masking metric, which I have labeled “outdoor” for convenience, even though it includes various non-residential indoor venues like offices, stores, or medical facilities. The resulting uncertainties would have biased the predicted effectiveness of masking toward the null.
[2] A latent variable, such as immune response or risky behavior, is a potential causal factor that cannot be directly observed. It can increase the need to explore a range of observable and potentially confounding variables.
