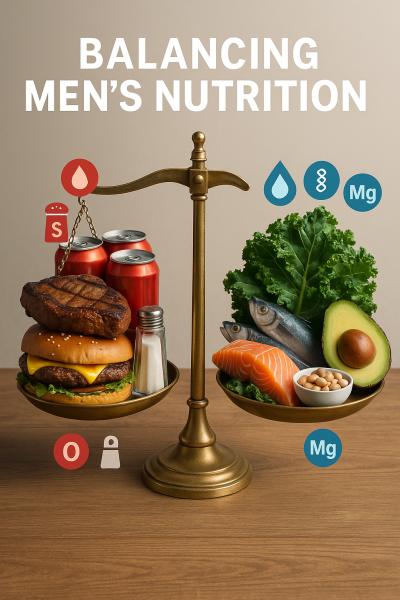
National surveys show men’s calorie and protein goals are usually met—often exceeded—but omega-3 fatty acids, vitamin D, fiber, and key minerals routinely fall short. As a result, men may be running a nutritional deficit even when their plate looks full. The turnaround? Simple swaps and eating more of the right food groups and nutrients can replace those excesses and fix the imbalances for good.
Eat More Plant Protein
Brings fiber and magnesium to the plate; helps solve the “too much animal protein” issue.
American men consume, on average, more protein from meat, poultry, and eggs than nutrition guidelines recommend—around 32 ounces per week (not including cured meats), compared with the 26 ounces that’s about right for a 2000 kcal daily intake pattern.
Sex differences in meat consumption emerge early: an analysis of more than 40,000 Americans found that by age five, boys already eat more meat than girls. This gap widens throughout adulthood, peaking in midlife (ages 51–65), when meat accounts for 3.5% more of men’s total food intake than it does of women’s.
This animal-heavy pattern leaves less room for nutrient-dense plant proteins that provide key nutrients men often lack—most notably magnesium (which supports muscle and nerve function, blood glucose regulation, and blood pressure) and fiber (important for digestive health).
Analysis of National Health and Nutrition Examination Survey (NHANES) data from 2013–2016 found that 48% of all Americans fall below their EAR (Estimated Average Requirement) for magnesium [1], with men aged 71 years and older and adolescent males among the most likely to have low intakes. Meanwhile, fiber intakes average only 17–18 grams daily—less than half the 38 grams per day recommended for men.
Spread protein across a variety of sources, including plant-based options such as beans, soy foods, nuts, and seeds. Switching to these proteins doesn’t just boost nutrient intake; it also trims saturated fat.
Pro tip: Swap half your 8-oz rib-eye steak for ½ can drained black beans. It adds about 8.7g of fiber and gives you about 62mg of magnesium compared with 38mg from the steak alone.
Eat More Oily Fish
Closes the omega-3 fatty acid gap in most men’s diets.
Within the broader “protein” category, seafood remains a weak link in the American diet, often sidelined when meat dominates the plate. Most men and women fall far short of recommended seafood intakes, leaving a persistent omega-3 deficit.
Omega-3 fatty acids are essential for heart and brain health, and in men may also support sperm quality. But data show that among men, the average intake of EPA and DHA —the biologically active omega-3s —is only about 102mg per day from foods, far below the 250mg per day provided when people consume the recommended intake of fish.
While men generally report slightly higher total fish intake than women, some analyses suggest they eat proportionally less of the oily types richest in EPA and DHA. Average intake of fish high in omega-3 fatty acids hovers around 1 ounce per week in men and women.
Fix it: Two 3-ounce servings of cooked fish per week, prioritizing oily types, [2] is the amount recommended by the American Heart Association. Meeting this target is a simple, evidence-backed way to support heart and metabolic health.
Pro tip: Not an oily fish fan? Start with milder options like salmon or trout before moving to stronger-flavored sardines or mackerel. Flake fish into pasta, tacos, or grain bowls—pairing with acid (lime, lemon, or tomato) plus herbs and spices helps tame “fishiness”.
Canned tuna is lower in omega-3s; other canned fish (e.g., salmon, sardines, mackerel) are much richer sources.
Consume More Potassium
Countering the downsides of excess sodium.
According to NHANES 2017–2020 data, the average sodium intake among U.S. men aged 19 plus is about 4,000mg per day—36% more than in women and around 75% more than the 2,300mg daily limit set by the Dietary Guidelines for Americans. Meanwhile, average potassium intake by men is about 2900mg per day—lower than the 3400mg recommended [3] for 19–50-year-old men.
This imbalance matters because sodium and potassium jointly regulate fluid balance, vascular tone, and nerve signalling. High sodium with low potassium intake causes blood vessel constriction and water retention, raising blood pressure. Increasing potassium promotes sodium excretion and relaxes blood vessels, reducing cardiovascular strain.
A few landmark analyses underscore potassium’s independent role in cardiovascular protection. A WHO-commissioned meta-analysis found that, in randomized trials, higher potassium intake reduced blood pressure, even without sodium reduction, especially in individuals with hypertension. In cohort studies, higher potassium was associated with a 24% lower stroke risk; the association with overall cardiovascular disease was directionally lower but not statistically significant.
Fix it: Aim to fill half your plate with potassium-rich produce—veggies, fruit, and legumes—and cook meals from fresh ingredients as often as possible instead of relying on sodium-heavy packaged foods. Potassium standouts include avocados, bananas, potatoes (including skin-on fries not drenched in salt), sweet potatoes, avocadoes, white beans, spinach.
Pro tip: If you need to season at home, use a sodium chloride/potassium chloride blend (such as Morton Lite Salt) instead of regular table salt (100% sodium chloride). Just check with your doctor first if you have kidney disease or take potassium-sparing medications.
Check in On Calcium and Vitamin D Intake
Keeping bones strong helps curb bone loss (which is not uncommon in men).
Osteoporosis isn’t just a women’s issue. Low bone mass, as measured at the hip or lower back, occurs in 27.5% of men aged 50-65 and 40.7% of men aged 65 and over, increasing fracture risk. When older men do break bones, they fare worse; hip fractures in males carry a higher one-year mortality rate than in women.
This is all the more reason to focus on calcium and vitamin D intake, which, along with weight-bearing and resistance exercise, help bones stay stronger longer. These nutrients work hand in hand: vitamin D enhances calcium absorption, while calcium supports bone structure, muscle contraction, and nerve function. Falling short on either may harm bone health, especially combined with other risk factors such as physical inactivity or heavy drinking.
For men, the RDA, or Recommended Dietary Allowance [4] for calcium intake is 1,000mg per day up to age 70 and 1,200mg per day afterward. Younger men, on average, meet the 1,000 mg calcium target, but intake drops off after age 70—even as needs rise. And those averages mask how widespread the shortfall is, with about one in four men aged 50–70 getting less than 780mg a day, and among those over 71, below 711mg.
For vitamin D, most men get about half their RDA, which is 10 micrograms (400 I.U.) per day. Sunlight can make up the difference—but not everywhere. In winter, regions north of the 37th parallel (roughly central California to southern Virginia) receive too little UVB radiation for the skin to produce adequate vitamin D.
Fix it: Don’t skip calcium-rich foods like milk and yogurt—three cups a day is the target—and round it out with other calcium sources such as leafy greens, almonds, and canned fish with bones. Most milk sold in the U.S. is fortified with about 3 micrograms (120 I.U.) of vitamin D per cup, so it can help you get your vitamin D too (also found in salmon, sardines, and eggs). In northern states during winter, consider a vitamin D supplement.
Pro tip: If you avoid dairy, choose fortified plant milks that provide added calcium and vitamin D to help fill the same gap.
Men’s diets often appear solid on the surface—plenty of calories, protein, and energy—but beneath that balance sheet lies a quiet deficit in nutrients that sustain long-term vitality. Magnesium, fiber, omega-3s, potassium, calcium, and vitamin D form the nutritional foundation for cardiovascular, muscular, and bone health, yet many men fall short. The good news is that these gaps are fixable with small, intentional shifts. It’s not about eating less, it’s about eating smarter.
[1] The Estimated Average Requirement (EAR): a nutrient intake value that is estimated to meet the requirement of half the healthy individuals in a group.
[2] This includes salmon, mackerel, herring, sardines, and trout
[3] Adequate Intake is defined as a best estimate of an amount assumed to ensure nutritional adequacy when there isn’t enough evidence to establish an EAR and RDA.
[4] Recommended Dietary Allowance (RDA): the average daily dietary intake level that is sufficient to meet the nutrient requirements of 97 to 98% healthy individuals in a group.



